GI CONDITIONS
get in touch with us
Abdominal Pain
Abdominal pain can manifest In a variety of ways, ranging from sharp or dull to chronic or intermittent.
Though abdominal pain is often due to an upset stomach or indigestion, it can also be caused by many possible health conditions that occur in the soft tissues and organs in your abdominal cavity.
Possible conditions that occur in the soft tissues and organs in your abdominal cavity. These are a few common causes of abdominal pain:
- Acid reflux
- Stomach virus
- Gallstones
- Kidney stones
- Gastric ulcer
- Diverticulitis
- Pancreatitis
- Appendicitis
- Celiac disease
- Crohn’s disease
- Cholecystitis
- Cirrhosis
Dr. Ashwath quickly performs an examination to determine if your pain represents an acute surgical abdomen, then proceeds with the complex task of determining the underlying cause.
You should seek immediate medical care for sudden, severe abdominal pain or if you had ongoing moderate pain that quickly worsened. These are signs of an acute abdomen that’s typically caused by an infection, inflammation, obstruction, or a blocked blood vessel.
Symptoms include:
- Fever
- Vomiting blood
- Ongoing nausea or vomiting
We begin with a thorough examination to learn about the type, location, severity, frequency, and duration of your pain. They also need to know if you have other symptoms, the foods you recently ate, and if certain movements make the pain better or worse. After performing a physical exam, your doctor may order blood tests, urinalysis or diagnostic imaging such as a CT scan. In some cases, your doctor may perform an upper endoscopy or colonoscopy to get a look at your digestive tract.
Treatment for abdominal pain depends on the underlying cause and the severity of your symptoms. There are many possible treatments for abdominal pain, ranging from medications and dietary changes to surges to treat bleeding, inflammation, blockages, stones, or tumours.
Acid Reflux /GERD
Acid reflux, or heartburn, happens to just about everybody from time to time. It occurs when stomach acid moves back up into your oesophagus through your lower esophageal sphincter.
If acid reflux feels uncomfortable and occurs regularly, you don’t have to suffer through it.
Common symptoms associated with acid reflux Include:
- A burning sensation in your chest or throat
- Heartburn
- Difficulty swallowing
- Wheezing or coughing
- A sour taste in your mouth
- Problems sleeping
- A hoarse voice
- The feeling of a lump in your throat
You might experience acid reflux after eating, when you lie down at night, during exercise, when you bend over or while wearing tight-fitted clothing. Being overweight and smoking increases your risk of acid reflux.
Eating a big meal or drinking coffee or alcohol might trigger symptoms or make them worse. Untreated acid reflux can cause esophageal damage or increase your risk of oesophageal cancer.
To help diagnose acid reflux, your gastroenterologist reviews your symptoms and medical history. They complete an exam and may use imaging tests or endoscopy to view the Inside of your digestive tract and rule out serious Gl complications.
Your acid reflux treatment plan is based on your health and the severity of your condition.
- Weight Loss – Losing weight if you’re overweight can reduce acid reflux. Your doctor helps you develop a healthy eating and exercise plan to get excess weight off.
- Dietary Changes – Eating certain foods can make acid reflux worse. Examples include spicy foods, greasy or fatty foods, onions, tomatoes, garlic, chocolate, alcohol, coffee and tea. Making dietary changes can offer you symptom relief.
- Lifestyle Changes – Additional lifestyle changes that can reduce acid reflux include not smoking, eating smaller meals, not eating right before bed, elevating the head of your bed and not wearing tight clothing.
- Medications – Taking over-the-counter or prescription medications can help reduce acid reflux symptoms. Your gastroenterologist will let you know which medicine is right for you.
- Surgery – If you have severe acid reflux that occurs regularly, your provider might recommend surgery to tighten your lower esophageal sphincter and give you long-lasting symptom relief.
Barett's Esophagus
Barrett’s esophagus is a condition in which the lining of your esophagus becomes irritated and is replaced by tissue normally found in your intestinal lining.
The condition is often caused by gastrointestinal esophageal reflux disease (GERD) and can increase your risk of esophageal cancer. Medical care from a specialist helps detect precancerous cells and offers you symptom relief.
It’s common not to experience symptoms associated with esophageal tissue changes and Barrett’s esophagus. However, if you have the condition, you might suffer from symptoms of GERD, including:
- Heartburn
- Chest burning or pain
- Problems swallowing food
The cause of Barrett’s esophagus isn’t entirely clear, but risk factors of the disease often include:
- Acid reflux
- Chronic heartburn
- Being white
- Being a man
- Smoking
- Being overweight or obese
In some cases, people with Barrett’s esophagus don’t have symptoms of acid reflux, and the cause of their condition isn’t known.
To diagnose Barrett’s esophagus, your gastroenterologist reviews your medical history and symptoms. They often complete an upper endoscopy, which Is a diagnostic procedure where your doctor uses a thin, lighted tube attached to a camera to view the Inside of your esophagus.
They may complete a biopsy during the procedure to make a final diagnosis.
- Useful Changes – If you have a mild case of Barrett’s esophagus, your doctor might recommend lifestyle changes to relieve GERD symptoms. Examples include weight loss, eliminating alcohol, coffee, chocolate, and other trigger foods, not smoking, avoiding tight clothes, and raising the head of your bed at night.
- Medications – Medications can relieve symptoms associated with GERD and Barrett’s esophagus. Your doctor lets you know which medicine best matches your needs.
- Routine Monitoring – Your doctor monitors Barrett’s esophagus using routine biopsies that can detect esophageal cancer.
- Minimally Invasive Procedures – For more severe cases of Barrett’s esophagus, your gastroenterologist might recommend minimally invasive procedures such as radiofrequency ablation, cryotherapy, or surgery to remove precancerous or cancerous cells In the esophagus.
Biliary Obstruction
Biliary obstruction stands as a complex facet within gastroenterology, demanding a meticulous examination to grasp its nuances. This blog post delves into the intricacies of biliary obstruction, elucidating its origins, clinical manifestations, diagnostic protocols, and therapeutic interventions.
Understanding biliary obstruction mandates a comprehensive grasp of the anatomical structures involved. The biliary system, encompassing the liver, gallbladder, and bile ducts, is essential for bile transport and digestion. Obstruction can occur at various points within this system, leading to a cascade of clinical implications.
A myriad of factors can precipitate biliary obstruction. Common culprits include gallstones, tumors, strictures, and inflammatory conditions. Recognizing the diverse etiologies is pivotal for accurate diagnosis and tailoring appropriate interventions.
Biliary obstruction manifests through a spectrum of clinical symptoms. Patients often present with jaundice, dark urine, pale stools, and abdominal pain. A meticulous assessment of these manifestations, coupled with a comprehensive patient history, aids in narrowing down the underlying cause.
Accurate diagnosis is fundamental in the management of biliary obstruction. Advanced imaging techniques, such as MRI, CT scans, and endoscopic procedures like ERCP, facilitate precise visualization of the biliary system. Understanding the extent and nature of the obstruction informs subsequent therapeutic decisions.
The management of biliary obstruction necessitates a tailored approach. While conservative measures such as medical therapies and dietary modifications may suffice in certain cases, more severe obstructions often warrant invasive interventions. Endoscopic stenting, balloon dilation, and surgical procedures constitute the armamentarium employed by gastroenterologists to alleviate obstruction and restore biliary flow.
In conclusion, biliary obstruction remains a multifaceted challenge in gastroenterology, demanding a systematic approach to unravel its complexities. Through an exploration of its anatomical foundations, causes, clinical manifestations, diagnostic methodologies, and therapeutic strategies, this blog post aims to equip both healthcare professionals and patients with a comprehensive understanding of this intricate gastroenterological concern. As we navigate the evolving landscape of gastrointestinal medicine, a nuanced comprehension of biliary obstruction becomes imperative for effective patient care.
Celiac Disease
Celiac Disease (CD) is a chronic digestive disorder characterized by inflammation of the small intestine, impacting nutrient absorption. This condition is triggered by the consumption of gluten, a protein found in wheat, barley, rye, and related grains. While oats are generally considered safe, the risk of contamination limits their recommended intake for those with CD.
Upon gluten ingestion, the immune system initiates an inflammatory response in the small intestine, damaging millions of finger-like projections called villi. These structures, crucial for nutrient absorption, become compromised, leading to decreased nutrient assimilation. Eliminating gluten from the diet reduces inflammation, allowing the intestine to heal gradually.
The onset of symptoms varies among individuals, with some experiencing effects decades after initial gluten exposure. Triggers can precipitate symptoms and signs, making the disease presentation diverse.
In the United States, an estimated 1 in 100 people may have CD, yet only 1 in 5 are diagnosed. CD spans various ethnicities, with Caucasians having the highest prevalence. While it can manifest in infancy, diagnosis often occurs in adulthood, with a higher incidence in females. Those with type 1 diabetes, thyroid disorders, or family history face an increased risk.
Symptoms vary widely, from mild inflammation with minimal signs to severe cases prompting medical attention. Common symptoms include abdominal pain, bloating, diarrhea, weight loss, anemia, and poor growth in children. CD can mimic other conditions, necessitating screening for patients with symptoms resembling irritable bowel syndrome.
The primary treatment for CD is adherence to a gluten-free diet, promoting intestinal healing. Dieticians play a crucial role in educating patients and tailoring gluten-free diets. Medications are rarely needed, except in cases where a gluten-free diet is ineffective. Support groups offer valuable resources for patients and their families.
- Gluten-Free Diet Guidelines: Avoiding gluten-containing grains like wheat, barley, rye, and related products is imperative. Patients must be vigilant label readers, identifying and eliminating potentially harmful ingredients. Certain grains and flours, labeled gluten-free, are safe alternatives.
- Lifelong Commitment: Once diagnosed, individuals must maintain a strict gluten-free diet throughout their lives. While the transition may be challenging initially, dieticians provide valuable support.
- Complications and Follow-Up: Non-adherence to the gluten-free diet leads to persistent symptoms and an increased risk of complications, including cancer and intestinal narrowing. Annual follow-ups, including blood tests and potential endoscopy, ensure ongoing healing and symptom resolution.
- Family Involvement: Given the genetic nature of CD, immediate family members should undergo testing, even if asymptomatic, to detect potential hidden cases
In conclusion, understanding Celiac Disease involves recognizing its diverse symptoms, adhering to diagnostic protocols, and committing to a lifelong gluten-free lifestyle. Regular follow-ups and family involvement are integral components of managing this chronic digestive disorder.
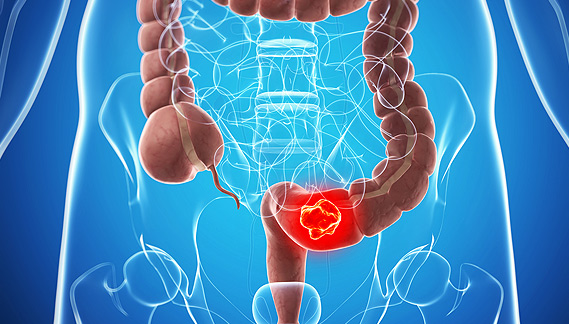
Cologuard®
Colorectal cancer is a prevalent health concern, but with advancements in medical technology, there are now more accessible and non-invasive screening options available. One such option gaining attention is Cologuard. In this section, we delve into the specifics of Cologuard and its significance in colorectal cancer detection.
Cologuard is a molecular stool test designed to detect both colorectal cancer and advanced adenomas. It employs advanced DNA analysis and fecal immunochemical testing to identify altered DNA and blood in the stool. Understanding the scientific basis of Cologuard is crucial for patients seeking an effective and convenient screening method.
While both Cologuard and colonoscopy serve as screening tools, they adopt distinct approaches and provide different information. Cologuard detects proteins shed from colon cancer and polyps, while colonoscopy visually identifies the polyps themselves.
Colonoscopy, despite its effectiveness, carries a low risk of complications, including reactions to sedatives or possible puncturing of the bowel. Cologuard, in contrast, eliminates these risks. However, a 2019 study identified limitations, including the potential for false negatives, overlooking larger polyps, and a higher risk of false positives compared to colonoscopies.
Notably, Cologuard and colonoscopy can complement each other in a screening regimen. Cologuard can serve as a non-invasive, first-line test for individuals at average risk, providing an additional layer of early detection.
The target demographic for the Cologuard test includes individuals at average risk, particularly those between 50 and 75 years old. Screening recommendations from the U.S. Preventive Services Task Force (USPSTF) suggest initiation at age 50, while the American Cancer Society recommends screening from age 45.
For individuals with an increased risk of colon cancer due to family history, inherited mutations, or other known risk factors, consultations with healthcare providers are vital. These discussions should explore the possibility of commencing screening even earlier.
Following the submission of a stool sample, Cologuard test results, delivered as either “negative” or “positive,” are sent to the attending physician. Negative results indicate the absence of atypical DNA or hemoglobin biomarkers, suggesting no signs of colon cancer or precancerous polyps. In the event of a positive result, further testing, typically a colonoscopy, is recommended to confirm and address potential issues.
It is crucial to acknowledge the presence of false positives and false negatives in Cologuard results. A 2014 clinical study revealed a 13 percent false positive rate and an 8 percent false negative rate, highlighting the importance of cautious interpretation.
In the ever-evolving landscape of colorectal health, Cologuard stands as a valuable addition to our arsenal of screening tools. Its non-invasive nature and accessibility contribute to increased screening compliance, potentially leading to earlier detection and intervention. However, maintaining a nuanced understanding of its benefits and limitations is paramount.
Constipation
Crohn’s disease is a chronic inflammatory bowel disorder that demands attention and understanding for those affected. This article aims to provide a concise yet comprehensive overview of Crohn’s disease, focusing on its definition, symptoms, diagnosis, treatment, and lifestyle management.
Constipation stands as a prevalent gastrointestinal woe in the United States and Western countries, prompting over 2.5 million annual doctor visits and substantial expenditures on laxatives. This article delves into the nuanced aspects of constipation, aiming to provide a comprehensive understanding of its definition, causes, diagnosis, treatment, and preventive measures.
Contrary to the common belief that daily bowel movements signify good health, constipation is not solely about frequency. The American College of Gastroenterology characterizes it by unsatisfactory defecation, encompassing infrequent stools, difficulty in passage, or a sense of incomplete evacuation. It’s crucial to consult a doctor if there’s a sudden change in bowel habits.
Constipation often results from slow stool movement through the digestive tract, influenced by factors such as low water intake, dietary changes, reduced physical activity, and certain medications. While infrequent, bowel obstruction can present a serious but uncommon cause.
A thorough diagnosis relies on patient history and physical examination. When uncertainty persists, additional tests, including sigmoidoscopy or colonoscopy, may be recommended. Tests like abdominal x-rays, capsule transit studies, anorectal manometry, and defecography might be employed to discern the root cause.
Addressing hard stool involves techniques such as tap water enemas, manual stool removal, and cleansing solutions. Subsequent steps include dietary adjustments, fiber supplementation, and occasional laxative use. Bulk-forming agents and osmotic agents play crucial roles, promoting softer stools and facilitating easier passage. Stimulant laxatives, though effective, are advised for short-term use and under supervision.
Prescription medications that enhance fluid secretion into the intestine are reserved for cases unresponsive to over-the-counter laxatives. In instances where constipation stems from opiate use, medications countering opiate effects on the gut may offer relief. Problems related to pelvic floor and anorectal muscle coordination may necessitate biofeedback or muscle retraining exercises, accessible through specialized centers and doctor referrals.
Combining adequate fluid intake, regular exercise, and a high-fiber diet proves beneficial in preventing constipation. Laxatives, particularly stimulant laxatives, can complement preventive measures, especially when faced with potentially constipating drugs.
In conclusion, understanding constipation involves navigating its multifaceted aspects, from defining symptoms to tailored treatment strategies. By embracing a holistic approach, individuals can effectively manage and prevent this common gastrointestinal concern. For further insights, consult a healthcare provider or book a visit with us.
Crohn's Disease
Crohn’s disease is a chronic inflammatory bowel disorder that demands attention and understanding for those affected. This article aims to provide a concise yet comprehensive overview of Crohn’s disease, focusing on its definition, symptoms, diagnosis, treatment, and lifestyle management.
The symptoms of Crohn’s disease vary in intensity and may include diarrhea, abdominal pain, fatigue, and the urgent need for bowel movements. Additional symptoms can range from weight loss to joint pain and skin issues. If persistent symptoms arise, seeking medical attention is crucial, as early detection is key to managing the disease effectively.
While the exact causes of Crohn’s disease remain unknown, genetics play a significant role. Individuals with a family history are more susceptible. Factors such as age, ethnicity, smoking, and NSAID use also contribute to the risk. Understanding these factors aids in early identification and proactive management.
Diagnosing Crohn’s disease involves a thorough examination of symptoms, medical history, and potential risk factors. Various tests, including blood tests, stool samples, imaging such as CT scans or MRI, and endoscopic procedures, help rule out other conditions and confirm the diagnosis. Early and accurate diagnosis sets the foundation for effective treatment.
Crohn’s disease has no cure, but its symptoms can be managed through medications, lifestyle changes, and, in some cases, surgery. Medications range from steroids to biologic therapies, tailored to each patient’s specific needs. Nutritional therapy and surgery may be considered in severe cases or when other treatments prove ineffective.
Living with Crohn’s disease involves adopting a healthy lifestyle, including a balanced diet, regular exercise, and smoking cessation for those who smoke. Collaboration with healthcare professionals, adherence to prescribed medications, and proactive management of symptoms contribute to a better quality of life.
In conclusion, understanding Crohn’s disease involves recognizing its signs, seeking timely medical evaluation, and actively participating in a comprehensive treatment plan. While living with a chronic condition presents challenges, a proactive and informed approach empowers individuals to manage their health effectively. If you suspect you may have Crohn’s disease or are at risk, consult with a healthcare provider for a personalized evaluation and guidance on managing this complex condition.
Diarrhea
Diarrheal diseases, both acute and chronic, represent a significant health concern in the United States and globally. This overview delves into the distinctions between acute and chronic diarrhea, their symptoms, causes, risk factors, and diagnostic approaches.
Acute diarrhea, ranking second only to respiratory infections in reported cases, is a prevalent ailment. It holds a prominent place in childhood mortality worldwide, particularly in developing nations. This form of diarrhea spans a duration of less than two weeks.
Characterized by loose or watery stools, acute diarrhea manifests with various associated symptoms such as abdominal cramps, fever, nausea, vomiting, fatigue, and urgency. Viruses, primarily rotavirus in children and norovirus in adults, are the leading culprits behind acute, watery diarrhea. Bacterial origins, notably in traveler’s diarrhea, also contribute to its prevalence.
Chronic diarrhea, persisting beyond four weeks, demands a comprehensive understanding. Its manifestations may include weight loss, malnutrition, abdominal pain, or other symptoms indicative of an underlying illness. Diverse causes underlie chronic diarrhea, categorized as fatty or malabsorptive, inflammatory, or predominantly watery. Conditions such as celiac disease, Crohn’s disease, and parasitic infections can lead to persistent gastrointestinal distress.
Infectious agents pose a major risk for acute diarrhea, often transmitted fecal-orally. Vigilant hand hygiene, especially with soap and water, plays a crucial role in prevention. Medications, recent dietary changes, and exposure to contaminated foods also contribute to the risk.
Acute Diarrhea: Most cases of acute diarrhea resolve without antibiotic therapy, but severe or persistent cases may require stool tests for bacteria and parasites. Blood tests aid in assessing fluid and electrolyte imbalances.
Chronic Diarrhea: Chronic cases necessitate a thorough diagnostic approach, including blood tests for anemia and infections, stool sample analysis, and endoscopic examinations to ascertain the etiology.
Acute Diarrhea: Fluid intake with sugar and salt is crucial to prevent dehydration during acute diarrhea. Specific dietary choices and, when necessary, anti-diarrheal drugs can aid symptom control.
Chronic Diarrhea: Treatment of chronic diarrhea depends on the identified etiology. Empiric treatment may be prescribed for symptomatic relief, with attention to replacing any mineral and vitamin deficiencies.
In addressing diarrheal diseases, a nuanced understanding of their distinctions, causes, and diagnostic pathways is pivotal. By incorporating preventive measures and tailored treatments, healthcare providers can effectively manage both acute and chronic cases, promoting improved patient outcomes.
Diverticular Disease
Diverticulosis and diverticulitis are gastrointestinal conditions that demand our attention, particularly as they become more prevalent, especially among the aging population. In this comprehensive overview, we delve into the intricacies of these conditions, exploring their definitions, causes, symptoms, diagnosis, prevention, complications, and treatment.
Diverticulosis is a prevalent condition characterized by the formation of small out-pouchings, known as diverticula, in the intestinal wall. These pouches, akin to “pot-holes” in the lining, are most commonly found on the left side of the large intestine, particularly in the descending and sigmoid colon. While the exact cause remains unclear, factors such as muscle spasms, genetic predisposition, and potential links to dietary fiber have been suggested.
Diverticulosis is notably common among older individuals, with a higher prevalence in those over the age of 60. Conversely, it is relatively uncommon in individuals under the age of 30.
The exact cause of diverticulosis remains elusive. Some theories propose that increased pressure in the colon, stemming from muscle spasms or straining, may lead to the formation of diverticula at weakened points in the colon wall. A genetic predisposition is also evident, implying a higher likelihood of developing diverticulosis if close family members have the condition. The role of dietary fiber in preventing or exacerbating diverticulosis remains a topic of debate.
While many individuals with diverticulosis are asymptomatic, some may experience left lower abdominal pain, a gassy sensation, or alterations in bowel habits. Diagnosis often involves procedures such as:
- Barium enema: X-ray imaging using liquid material to highlight the colon’s outline.
- Colonoscopy: Visual examination of the colon using a flexible tube equipped with a camera.
- CT scan: Multiple x-ray images providing a comprehensive view of the body.
Lifestyle and Dietary Measures
While the prevention of diverticulosis remains uncertain, maintaining a healthy weight, avoiding smoking, and incorporating a high-fiber diet may contribute to overall colon health. Contrary to previous beliefs, recent studies suggest that restricting foods like popcorn, nuts, and seeds may not be necessary for individuals with diverticulosis.
Medications and Recurrent Diverticulitis
Various medications have been explored to prevent recurrent diverticulitis, but their efficacy remains inconclusive. Mesalamine, a well-studied drug, has not demonstrated significant success in reducing the likelihood of recurrent episodes. Limited studies on probiotics and rifaximin, an antibiotic, warrant further investigation to determine their potential benefits.
Diverticulitis Complications
Diverticulitis, inflammation of diverticula, can lead to complications such as abscess formation, stricture, fistula, and perforation, the most serious of all. Additionally, diverticular bleeding may occur, characterized by the sudden passage of significant amounts of blood.
Treatment Strategies
Treatment typically involves antibiotics and a light diet. Mild cases may be managed without antibiotics, while severe cases or those with complications necessitate hospitalization and, in some instances, surgical intervention. X-ray-guided drainage and surgery become viable options for managing complications or unresponsive cases.
In conclusion, understanding diverticulosis and diverticulitis involves a multifaceted approach encompassing awareness, lifestyle adjustments, and tailored medical interventions. Regular medical check-ups and early intervention can significantly contribute to managing and preventing complications associated with these conditions.
Eosinophilic Esophagitis
Eosinophilic esophagitis (EoE) is an allergic condition characterized by inflammation in the esophagus, impacting individuals with specific allergies, asthma, or eczema. This chronic condition is increasingly prevalent, particularly among young men, necessitating continuous management to alleviate symptoms.
Eosinophilic esophagitis, or EoE, manifests as elevated levels of eosinophils—white blood cells—in the esophageal tissue. This heightened presence results in inflammation, leading to symptoms such as chest pain, heartburn, difficulty swallowing, and food impaction.
While there is no cure for EoE, proper treatment allows individuals to function well and maintain their quality of life. The focus lies on symptom management, acknowledging the chronic nature of the condition.
Symptoms vary across age groups, encompassing difficulty feeding and poor growth in infants, abdominal pain and swallowing difficulties in children, and heartburn and chest pain in adults. Recognizing these signs is crucial for timely intervention.
EoE diagnosis involves a thorough evaluation, starting with a patient’s medical history and symptoms. Upper endoscopy, accompanied by biopsy, confirms the presence of eosinophils and rules out other conditions. Risk factors, including gender, allergies, asthma, and family history, increase susceptibility.
Treatment for EoE revolves around dietary changes and medications. Elimination and elemental diets aid in identifying allergens, while acid-blocking medications and topical corticosteroids manage inflammation. Esophageal dilation is an option for those with strictures. Ongoing research explores newer medications targeting the immune system.
Individuals with Eosinophilic Esophagitis can lead fulfilling lives with proper management. Regular consultation with a healthcare professional is essential for accurate diagnosis, personalized treatment plans, and minimizing the risk of complications. Understanding the intricacies of EoE empowers individuals to proactively address their health concerns and seek timely medical intervention.
GallBladder Disorders
In the intricate realm of gastrointestinal health, the gallbladder assumes a pivotal role in the digestion process. This blog post endeavors to unravel the complexities of gallbladder disorders, providing insights into their causes, symptoms, and potential treatment modalities.
Gallbladder disorders manifest in a spectrum of conditions, each presenting distinctive challenges. Predominantly, gallstones, crystallized bile components causing obstruction and discomfort, stand as the most prevalent disorder. Concurrently, inflammation of the gallbladder (cholecystitis) and biliary dyskinesia, characterized by impaired gallbladder contraction, constitute commonly encountered issues.
Timely intervention hinges on heightened awareness of symptoms. Patients with gallbladder disorders typically experience abdominal pain, especially postprandial pain following high-fat meals, along with nausea, vomiting, and in severe cases, jaundice. It is imperative to recognize that symptoms may vary, necessitating professional evaluation for an accurate diagnosis.
The cornerstone of effective management lies in accurate diagnosis. Utilizing advanced diagnostic modalities such as ultrasound, CT scans, and HIDA scans empowers clinicians to visualize the gallbladder, identifying abnormalities. Precision in understanding the disorder’s nature is crucial for tailoring an appropriate treatment plan.
Gallbladder disorder management spans from lifestyle adjustments to surgical interventions. Dietary modifications, including a low-fat diet, often suffice to manage symptoms. Surgical removal of the gallbladder (cholecystectomy) becomes a consideration when conservative measures prove inadequate. This decision is individualized, considering symptom severity and overall patient health.
Gallbladder disorders present formidable challenges to digestive health, demanding a comprehensive understanding for effective management. This exploration of anatomy, disorders, symptoms, diagnostics, and treatments seeks to empower individuals with knowledge, fostering informed discussions with healthcare providers. As the field of gastroenterology evolves, staying abreast of advancements is pivotal for digestive well-being.
Gastritis and Ulcers
Gastritis and ulcers, though common, remain misunderstood by many. Let’s delve into the intricacies of these gastrointestinal conditions. Gastritis involves the inflammation of the stomach lining, while ulcers signify open sores in the stomach lining or the upper part of the small intestine. Understanding the fundamental characteristics of these ailments is crucial for informed healthcare decisions.
To comprehend gastritis and ulcers, one must explore their root causes. Helicobacter pylori (H. pylori) infection, long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs), excessive alcohol consumption, and stress are among the primary contributors. Unraveling the complexities of these causative factors is paramount in crafting effective treatment plans.
Accurate diagnosis is the linchpin for effective intervention. Gastroenterologists employ an array of diagnostic tools, including endoscopy, blood tests, and imaging studies, to identify and characterize gastritis and ulcers. Precise diagnosis lays the groundwork for tailored treatment strategies, enhancing patient outcomes.
Armed with a comprehensive understanding of the patient’s condition, gastroenterologists can employ targeted treatment approaches. This may include medications to neutralize stomach acid, antibiotics for H. pylori eradication, and lifestyle modifications. Crafting personalized treatment plans ensures a more nuanced and effective response to the individual patient’s needs.
Preventing the recurrence of gastritis and ulcers requires a multifaceted approach. Gastroenterologists often advocate for lifestyle modifications, such as dietary changes, stress management, and prudent use of medications. By embracing preventive measures, individuals can actively participate in maintaining their gastrointestinal health.
In conclusion, demystifying gastritis and ulcers is pivotal in fostering a proactive approach to gastrointestinal well-being. From understanding the basics to exploring diagnostic methodologies and treatment modalities, this overview aims to empower individuals with knowledge, enabling them to navigate the complexities of these prevalent conditions. By fostering awareness and promoting informed decision-making, we pave the way for a healthier, more resilient digestive system.
Hemorrhoids
The rectum, the final portion of the colon, serves as the conduit for expelling stool through the anus. While ailments in this region are prevalent, societal discomfort often inhibits open discussions with healthcare providers. Recognizing symptoms like bleeding, pain, and itching is crucial, prompting the need for professional consultation.
Hemorrhoids, engorged blood vessels in the rectum or anal canal, manifest through symptoms such as rectal bleeding. Surprisingly common, with almost half of Americans experiencing them by age 50, these conditions often go unreported. External hemorrhoids, discernible as protrusions near the anus, may cause pain when swollen. Conversely, internal hemorrhoids, situated inside the rectum, can occasionally protrude.
While external hemorrhoids may remain asymptomatic, internal ones might lead to painless rectal bleeding. Straining during bowel movements, stemming from conditions like constipation or diarrhea, can contribute to hemorrhoid development. Pregnancy and heavy lifting, increasing abdominal pressure, also elevate the risk.
Prompt diagnosis relies on attentive examination. External hemorrhoids are observable during an anal examination, while internal ones may necessitate tools like a sigmoidoscope or anoscope. Initial treatment involves lifestyle adjustments, including adequate fluid intake, fiber supplements, and stool softeners. Soaking in a warm bath or using over-the-counter creams often proves effective.
For persistent cases, medical interventions range from rubber band ligation to surgical procedures. These approaches aim to alleviate discomfort and rectify recurrent issues.
Hiatal Hernia
Hiatal hernia, a common yet often misunderstood gastrointestinal condition, occurs when a portion of the stomach protrudes through the diaphragmatic hiatus into the chest cavity. This displacement of the stomach can lead to a range of symptoms, making it imperative to delve into the intricacies of this condition.
To comprehend the nuances of hiatal hernia, one must scrutinize its origins. The primary cause lies in the weakening of the diaphragmatic hiatus, allowing the stomach to breach its normal anatomical position. Contributing factors include age-related changes, obesity, and increased abdominal pressure from factors such as persistent coughing or heavy lifting.
Recognizing the symptoms of hiatal hernia is crucial for timely intervention. While some individuals may remain asymptomatic, others may experience heartburn, regurgitation, chest pain, or difficulty swallowing. Accurate diagnosis often involves a combination of medical history assessment, physical examination, and diagnostic imaging techniques such as endoscopy or barium swallow.
In addressing hiatal hernia, a tailored approach is essential. Lifestyle modifications, including weight management and dietary adjustments, are often the initial recommendations. Medications may provide symptomatic relief, while surgical intervention becomes a consideration for cases resistant to conservative measures. A comprehensive evaluation by a gastroenterologist is paramount to determine the most suitable course of action.
Preventing the occurrence or recurrence of hiatal hernia involves adopting a mindful lifestyle. Maintaining a healthy weight, practicing good posture, and refraining from overeating are key preventive measures. While many individuals can manage hiatal hernia effectively with conservative measures, understanding the long-term prognosis is crucial for informed decision-making regarding treatment options.
In conclusion, comprehending the intricacies of hiatal hernia is fundamental for both healthcare professionals and individuals alike. This condition, while common, necessitates a nuanced understanding of its causes, symptoms, and appropriate management strategies. By delving into these aspects, individuals can empower themselves with knowledge to navigate the complexities of hiatal hernia effectively.
Irritable Bowel Syndrome
When it comes to managing Irritable Bowel Syndrome (IBS), understanding the symptoms and exploring effective treatment options is crucial. The American College of Gastroenterology (ACG) provides comprehensive guidelines to assist both patients and doctors in making informed decisions for symptom management.
Despite IBS affecting 10-15% of adults in the United States, only 5-7% receive a formal diagnosis. The range of symptoms includes constipation, characterized by infrequent and challenging bowel movements, and abdominal pain, a prevalent issue often associated with IBS. ACG’s guidelines serve as a valuable resource for tailored approaches to symptom management.
Defined as a condition causing abdominal pain and irregular bowel movements, IBS affects 10-15% of the U.S. population, with a higher prevalence in women. While lifelong and challenging to manage, IBS doesn’t pose a risk of serious conditions like colon cancer. Understanding its symptoms, including belly pain, gas, and altered bowel movements, is crucial for effective management.
The exact cause of IBS remains elusive, though it’s linked to changes in nerves and muscles controlling gut sensation. Stress and anxiety exacerbate symptoms but do not cause IBS. While its origins may trace back to bowel infections or microbial imbalances, IBS is not associated with food allergies. Seeking medical attention is crucial for accurate diagnosis and personalized treatment.
Managing IBS involves lifestyle adjustments, dietary modifications, and stress reduction. Avoiding trigger foods, incorporating soluble fiber, and seeking psychological support are integral components of symptom management. While there’s no cure, medications targeting specific symptoms, such as peppermint oil for pain or anti-diarrheal drugs, provide relief for many patients.
IBS is a real medical condition affecting 10-15% of the U.S. population. Symptoms disrupt daily life and may include abdominal pain, bloating, diarrhea, and/or constipation. Seeking care and exploring new therapies offer hope for restoring a better quality of life.
In conclusion, understanding IBS, its symptoms, and available resources empowers individuals to manage their condition effectively. With ongoing research and collaborative efforts, the journey toward improved IBS management continues, offering realistic hope for those impacted by this prevalent gastrointestinal disorder.
Liver Disease
Liver diseases encompass a broad spectrum of conditions, each presenting unique challenges to individuals and healthcare professionals. In this comprehensive exploration, we delve into the intricate landscape of liver diseases, shedding light on their varied facets, causes, and potential interventions.
As the largest internal organ, the liver engages in complex metabolic functions crucial to life. Understanding its role in processing nutrients, bile production, and blood protein synthesis is foundational to grasping liver diseases. The liver’s involvement in processing blood from the digestive system is pivotal. Recognizing its intricate vascular system provides insights into the development and progression of liver diseases.
Hepatitis Variants: Viral Onslaughts
Exploring hepatitis variants (A, B, C, D, and E) provides insights into their distinctive features, transmission modes, and the evolving landscape of vaccinations and antiviral therapies.
Fatty Liver Disease: An Emerging Epidemic
Non-alcoholic fatty liver disease (NAFLD) and alcoholic liver disease (ALD) pose growing health concerns. Examining their causes, risk factors, and potential consequences is crucial in addressing this burgeoning issue.
Cirrhosis and Beyond: Scarring Consequences
Cirrhosis, resulting from long-term liver injury, is a focal point. Yet, the intricate interplay of diverse causes, including alcohol use, viral infections, fatty liver disease, and autoimmune conditions, highlights the complexity of this condition.
Radiological tools, liver biopsy, and emerging diagnostic approaches contribute to a nuanced understanding of liver diseases. Evaluating their merits aids in precise diagnosis and targeted interventions.
Early non-specific symptoms, including fatigue and itching, often serve as initial clues. Recognizing the varied manifestations, such as edema, ascites, bleeding, jaundice, and hepatic encephalopathy, is crucial for timely intervention.
Pharmacological approaches, lifestyle modifications, and disease-specific interventions form the crux of managing liver diseases. Tailoring strategies based on the underlying cause is essential for effective patient care. Unraveling prognostic factors, ongoing research, and emerging therapies offer a glimpse into the future of hepatology. While advancements provide hope, recognizing the challenges ahead is integral to shaping improved outcomes.
In the intricate realm of liver diseases, awareness, understanding, and proactive management are paramount. This exploration serves as a guide for both healthcare professionals and individuals, fostering a holistic approach to liver health amidst the diverse array of hepatic challenges.
Microscopic Colitis
Microscopic colitis, though lesser-known, is a significant gastrointestinal condition that warrants attention and understanding. This article delves into the key aspects of microscopic colitis, providing a comprehensive overview for those seeking insights into this condition.
Microscopic colitis is characterized by chronic, watery diarrhea, and inflammation of the colon mucosa that can only be identified through microscopic examination. The diagnosis involves analyzing tissue samples obtained through colonoscopy or sigmoidoscopy. A thorough understanding of the diagnostic process is essential for healthcare practitioners and patients alike.
There are two primary types of microscopic colitis: collagenous colitis and lymphocytic colitis. Collagenous colitis is marked by a thickened band of collagen in the colon lining, while lymphocytic colitis is distinguished by an increased number of lymphocytes in the mucosa. Recognizing these distinctions is pivotal in tailoring treatment approaches to individual patients.
Patients with microscopic colitis often present with chronic diarrhea, abdominal pain, and weight loss. While the symptoms may overlap with other gastrointestinal disorders, understanding the unique clinical presentation of microscopic colitis is crucial for accurate diagnosis and prompt intervention.
Management of microscopic colitis involves a combination of lifestyle modifications and pharmacological interventions. Medications such as budesonide have shown efficacy in controlling inflammation and providing symptomatic relief. Awareness of the available treatment options empowers both healthcare professionals and patients in navigating the complexities of managing this condition.
Microscopic colitis is generally considered a benign condition; however, its impact on an individual’s quality of life should not be underestimated. Exploring the long-term prognosis and potential advancements in research opens avenues for enhanced patient care and improved outcomes.
In conclusion, understanding microscopic colitis requires a multifaceted approach that encompasses diagnosis, classification, clinical presentation, treatment strategies, and future considerations. This article serves as a primer for healthcare professionals and individuals seeking comprehensive insights into this intriguing yet often overlooked gastrointestinal condition. Through continued research and awareness, we can better navigate the nuances of microscopic colitis and offer optimized care to those affected.
Pancreatitis
The pancreas, a relatively inconspicuous organ nestled behind the stomach, assumes a pivotal role in our physiological equilibrium. Often overshadowed by its silent function, the pancreas becomes the focus when anomalies arise, leading to conditions such as pancreatitis, pancreatic cysts, or pancreatic cancer.
At the crossroads of digestion and metabolic control, the pancreas orchestrates the secretion of enzymes vital for nutrient breakdown and hormones like insulin, crucial in regulating blood sugar levels. Understanding the dual nature of this organ lays the groundwork for comprehending the disruptions that manifest as pancreatitis.
Acute pancreatitis, marked by sudden inflammation, manifests in diverse etiologies, including gallstones, alcohol abuse, and various metabolic factors. This section outlines the diagnostic criteria, emphasizing the amalgamation of symptoms, physical examination, and laboratory tests. Imaging studies such as computed tomography (CT) scans serve as crucial tools for precise diagnosis.
The symptoms of acute pancreatitis, a painful ordeal marked by abdominal distress, nausea, and vomiting, demand prompt attention. This section delineates the characteristic symptoms, facilitating early identification and intervention.
Chronic pancreatitis, a sequel to ongoing inflammation, heralds irreversible damage, impacting digestion and blood sugar control. Recognizing the symptoms, including chronic abdominal pain, steatorrhea, and weight loss, becomes paramount in managing this persistent condition. Furthermore, the inextricable link between chronic pancreatitis and pancreatic cancer warrants regular screenings.
This section elucidates the distinct treatment approaches for acute and chronic pancreatitis. Hospital admission, pain management, nutritional interventions, and, in severe cases, surgical interventions form the crux of acute pancreatitis management. Chronic pancreatitis, on the other hand, necessitates a multifaceted approach, encompassing pain relief, enzyme supplementation, and lifestyle modifications such as abstinence from alcohol and tobacco.
In conclusion, unraveling the complexities of pancreatitis provides a roadmap for both patients and healthcare practitioners. Timely intervention, coupled with comprehensive lifestyle adjustments, emerges as the linchpin in mitigating the impact of pancreatitis and preventing its recurrence. Understanding the nuances of this intricate interplay between organ, dysfunction, and treatment arms individuals with the knowledge needed to navigate the challenges posed by pancreatitis.
Rectal Pain & Bleeding
The rectum, the last segment of the digestive tract, plays a crucial role in maintaining our digestive health. Despite the prevalence of rectal problems, a significant number of adults hesitate to seek medical advice due to embarrassment. This article aims to provide a thorough understanding of common rectal issues, emphasizing the importance of early recognition and proper diagnosis.
Hemorrhoids, akin to varicose veins in the legs, can become swollen or stretched. They manifest in two types: external, visible under the skin, and internal, originating inside the rectum. The development of hemorrhoids is often linked to increased pressure during bowel movements, pregnancy, constipation, diarrhea, genetic factors, and aging. Diagnosis involves visual examination, rectal examination, and sometimes anoscopy or sigmoidoscopy. Medical treatment focuses on softening bowel movements, topical creams, sitz baths, and dietary adjustments.
Various procedures exist for treating hemorrhoids. These include banding (placing a rubber band to induce strangulation and scarring), sclerotherapy (injection of a chemical solution to shrink hemorrhoids), infrared coagulation (using a device to destroy internal hemorrhoids), radiofrequency ablation (employing high-intensity sound waves to close off hemorrhoids), and hemorrhoidectomy (surgical removal of hemorrhoid veins, typically requiring hospitalization).
An anal fissure is a common condition involving a tear in the lining of the anal canal. Diagnosis is achieved through a painful digital examination, external inspection, or anoscopy. Treatment involves prevention through a high-fiber diet, sitz baths, stool softeners, and topical creams. Surgical intervention may be necessary if symptoms persist.
Anal abscesses, pus-filled cavities, and fistulas, connections or tunnels between the anal gland and buttocks, present with symptoms such as pain, swelling, and fever for abscesses and drainage for fistulas. Medical options exist for abscesses caused by underlying conditions like Crohn’s disease, while surgical options involve cutting the sphincter muscle.
Fecal incontinence, characterized by the accidental loss of stool, has various causes. Evaluation methods include anorectal examination, digital examination, anal manometry, X-rays, and ultrasound. Treatment options range from dietary modification and medicines to biofeedback and surgery, depending on the underlying cause.
Pruritus ani, itching around the anal area often aggravated by excessive cleaning, can have causes such as excessive cleaning, sweating, certain beverages, and rarely infections or skin conditions. Treatment involves avoiding irritating soaps, blotting the area gently, eliminating irritating foods, and considering protective pastes.
In conclusion, understanding and addressing rectal problems promptly can lead to effective management and improved quality of life. It is crucial to overcome the stigma associated with these issues and prioritize one’s health. Always consult a healthcare professional for an accurate diagnosis and tailored treatment plans.
